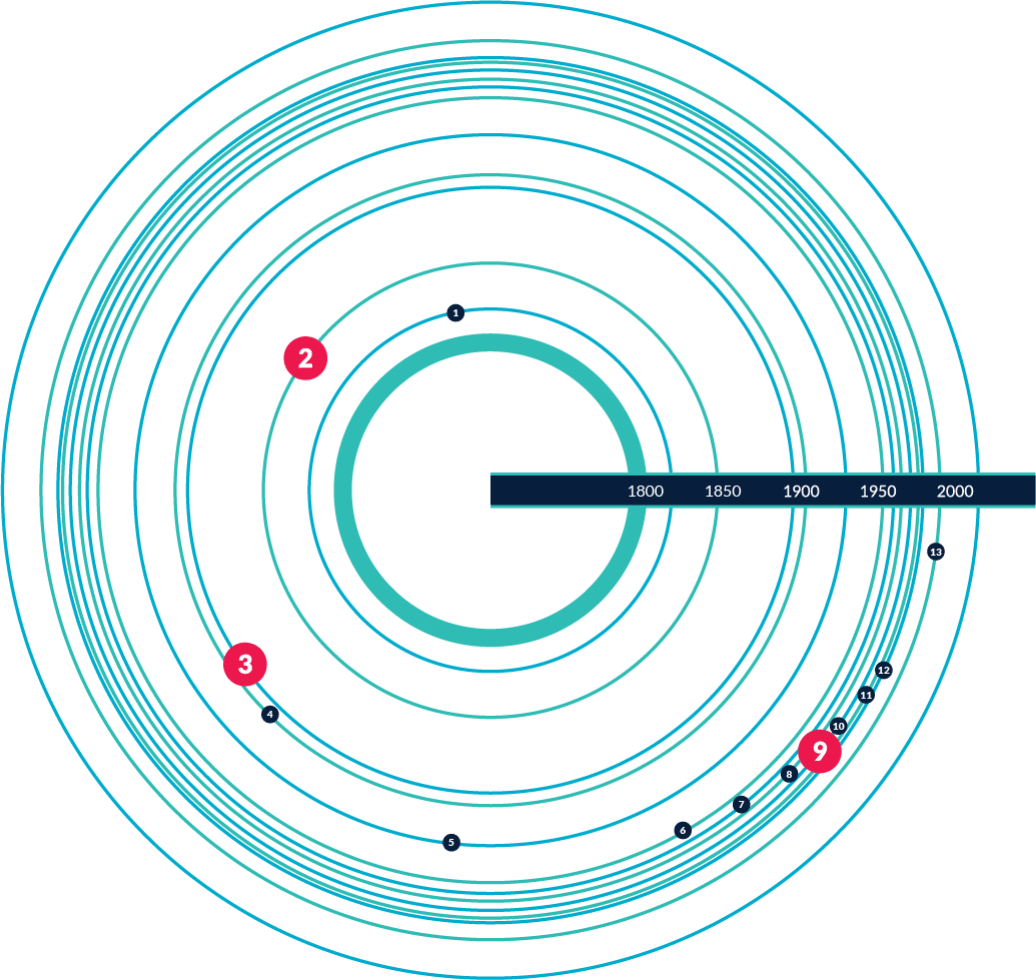
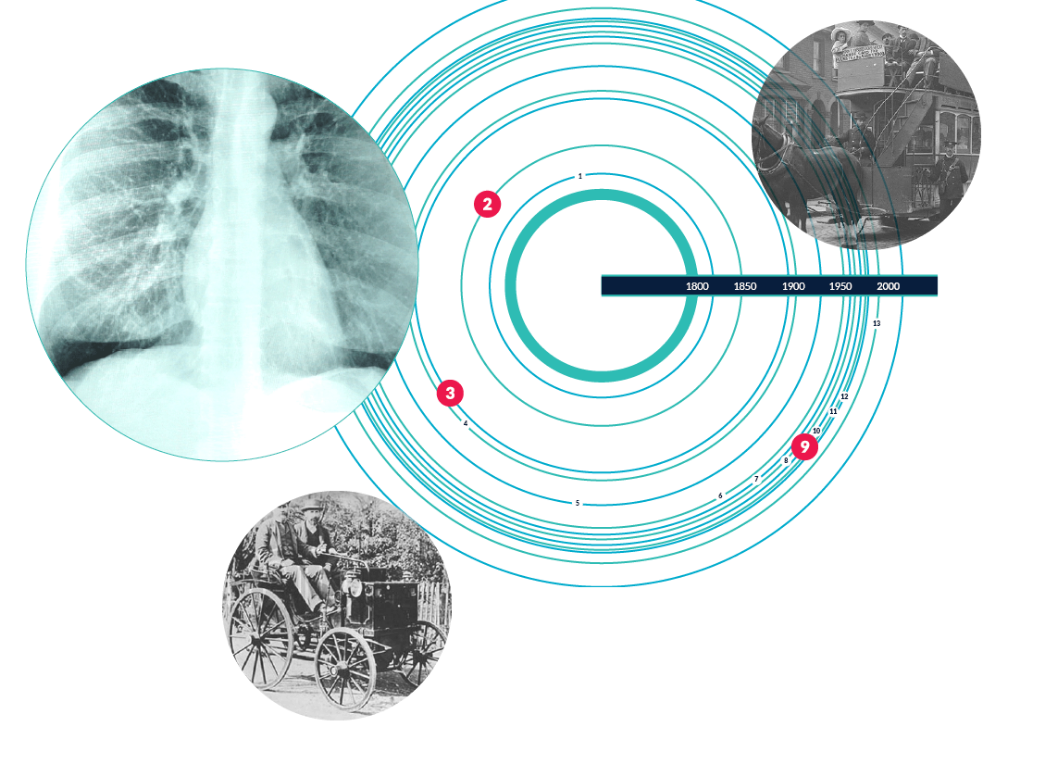
Current gold star lung diagnostic tools are inadequate for many patients. Nearly all lung pathologies are associated with regional changes in airflow throughout the lungs at onset of disease. Yet the current gold standard diagnostics yield average results over the entire lung – and for loss of total lung function to be measurable, local disease must be advanced. It is critical to detect even subtle functional losses well before lung structure is irreversibly affected by disease - in all lung locations and throughout the respiratory cycle - so that treatment is applied earlier.
What are the current modalities? Why are they inadequate for children, adults and the very sick?
How is it also inadequate for children, elderly & the very sick?
• Due to ionizing radiation dose, the use of X-ray based techniques (especially CT) for detection and treatment of acute respiratory disease is severely restricted for children
• Current scanning techniques require a patient to follow instructions and remain
still. While that presents an
extreme obstacle for
imaging small children
under the age of six, it is
a near-impossibility to
scan infants which has
led to the development
of instruments such as
the one shown here

• Limited mobility poses significant challenges for imaging the very sick and/or elderly
• Patients with chronic lung disease have a greater difficulty breathing when lying
horizontally. This makes the scanning
experience extremely
uncomfortable
for the
patient, but also
forces
them to exert much
more effort to breathe
than they normally
would

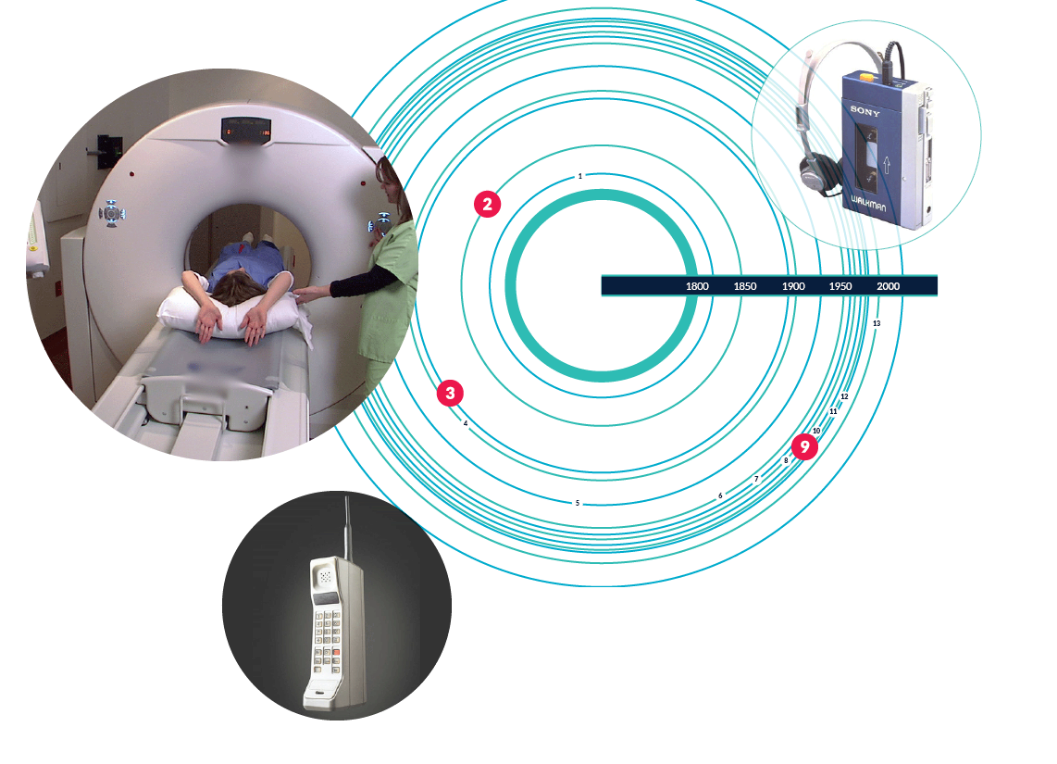
Spirometry Invented in 1846 by physician, John Hutchinson to measure how much air you inhale, how much you exhale, and how quickly you exhale.
Pros: Key benefit is that it measures functionality
Cons: -
Measurements are one-dimensional and are not region-specific - For lung function loss to be detected, disease must be significantly advanced